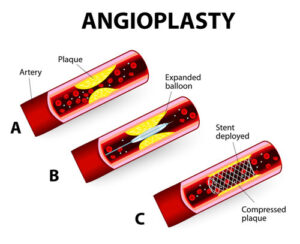
“Angioplasty” refers to the process of stretching an artery that is obstructed or narrowed using a balloon. Two main components often involved in this procedure are the angioplasty balloon and the stent. Here we’ll discuss the difference between an angioplasty balloon vs stent.
What is balloon angioplasty?
It is important to note that there are several types of angioplasty procedures, including angioplasty stenting and angioplasty ballooning. To put it simply, an angioplasty is a surgical treatment used to improve the flow of blood to and from the heart.
A little balloon is attached to the end of a cardiac catheter in order to perform balloon angioplasty. Plaque condenses when the balloon is gradually inflated to strain the arterial wall. An increase in inner artery diameter is the outcome.
The surgeon will next gently deflate and remove the balloon after the artery is open. In the next weeks, the patient will need to be observed to make sure the artery stays open and blood flows to and from the heart as it should.
What is a stent?
Stent procedures are often used in conjunction with balloon angioplasty; in fact, approximately 80% of patients who undergo balloon angioplasty will also have a stent placed.
The purpose of the stent is to act as a scaffold or support, keeping the vessel open, which helps to improve blood flow to the heart muscle and reduce the pain of angina.
There are two main types of stents:
- Bare-metal stents (BMS): These stents are simple metallic frameworks that prevent immediate recoil of the artery after angioplasty.
- Drug-eluting stents (DES): These stents are coated with medication that is gradually released to prevent tissue growth and re-narrowing of the artery.
Here’s a table highlighting the key differences between Angioplasty Balloon vs Stent:
| Criteria | Angioplasty Balloon | Stent |
| Definition | A medical procedure where a balloon is used to temporarily widen a narrowed artery. | A small wire mesh tube placed in an artery to keep it open after angioplasty. |
| Usage | Used to open blocked or narrowed arteries by inflating a balloon at the blockage site. | Used to permanently support the artery after the balloon has been deflated and removed. |
| Duration of Effect | Temporary; the artery may narrow again after the balloon is deflated and removed (restenosis). | Permanent; stays in place to prevent the artery from narrowing again. |
| Material | Plastic balloon attached to a catheter. | Metal (usually stainless steel or cobalt-chromium alloy). |
| Re-narrowing Risk (Restenosis) | Higher risk if used alone without stent placement. | Lower risk due to its permanent placement and drug-eluting options. |
| Types | Balloon angioplasty. | Bare-metal stents (BMS) or drug-eluting stents (DES). |
| Procedure Complexity | Simpler and quicker, but with potential for restenosis. | Slightly more complex due to permanent implant placement. |
| Recovery Time | Shorter compared to stent placement, but may require follow-up if restenosis occurs. | Longer recovery due to the permanent nature of the stent, but more effective in the long term. |
| Long-term Outcome | May require repeated procedures if artery narrows again. | Better long-term outcomes in terms of preventing re-narrowing. |
Important distinctions between angioplasty balloon vs stent:
Nature of Treatment
Balloon Angioplasty: Mostly used to compress plaque and temporarily widen the artery.
Stent: Supports the artery and prevents blockages from occurring in the future, offering a more long-term treatment.
Risk of Restenosis:
Balloon Angioplasty: 30–40% of instances result in re-narrowing; higher risk of restenosis.
Stent: Much decreased risk of restenosis, particularly when combined with drug-eluting stents, which cut the rate of re-narrowing to 5–10%.
Procedures:
Balloon Angioplasty: Less invasive and quicker, but may not provide long-term results.
Stent: Involves inserting a foreign item into the artery; although it provides longer-lasting advantages, there is a chance of problems including clotting or stent failure.
Drugs:
Balloon Angioplasty: If only a balloon is utilized, patients may not need long-term antiplatelet medication.
Stent: In order to lower the risk of clot formation surrounding the stent, patients must take blood-thinning medications.
Conclusion:
Angioplasty balloon vs stent have both shown to be vital weapons in the battle against coronary artery disease. Stents provide a more long-lasting treatment, particularly for patients who are at risk of restenosis, whereas balloon angioplasty provides a rapid and efficient means of removing blockages. In order to choose the optimal course of therapy for their unique circumstances, patients should consult extensively with their cardiologists, considering the short- and long-term risks and advantages of each option.

